Best Maryland Dispensary
For Medical + Recreational THC Products
We prioritize medical patients. A valid government-issued ID is required for those 21 and older, except for medical patients aged 18 and older.
One-Stop CannaShop
Our Germantown Dispensary THC Products
What makes the best Maryland dispensary? It’s top-shelf cannabis, high-quality accessories, and a great team. Infused together we create a one-stop-cannashop experience true to Maryland's cannabis culture.

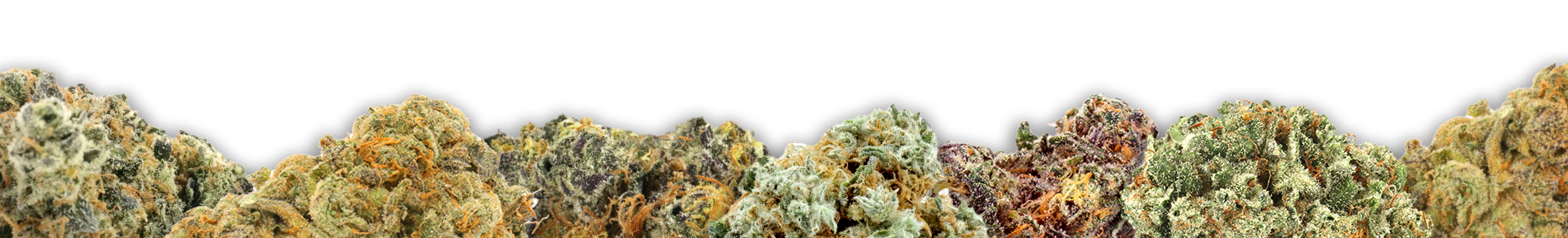
Flower

Pre-Rolls

Vape Carts

Concentrates

Edibles

Transdermals

Sublinguals

Accessories
Find Us in Germantown, MD
Monday - Sunday: 9:00am - 9:00pm
11530 Middlebrook Road Germantown, MD 20876
(240) 813-8818
Monday - Sunday:
9:00am - 9:00pm
11530 Middlebrook Road Germantown, MD 20876
(240) 813-8818
MoCo’s Nearby Dispensary
Proud to be the first cannabis dispensary to open in Germantown back in 2018, we are honored to be able to grow our roots within the MoCo community. Our goal from day one has been to find the best cannabis in Maryland and infuse it with the greatest Marylanders creating our very own entourage effect which we call the Bloom Experience. We are located in Middlebrook Square next to the Navy Federal Credit Union with entrances to our store via Frederick Rd and Middlebrook Road. Just 3 min away from Montgomery College and the Earthoid Water Tank.